Aarav ASD Device
Kriti DCMP
Sukhmani PDA Device

Utkarsh PDA Device
ASD (Atrial Septal Defect) Device Closure (Angiographically without Heart Surgery)
Three patients underwent successful ASD device closure angiographically without heart surgery. Patients were from Iraq, Myanmar and Delhi.
VSD (Ventricular Septal Defect) Device Closure (Angiographically without Heart Surgery)
Four years old child from Delhi underwent successful VSD device closure with no complications.
Atrial Septal Defect (ASD) Surgical Closure
Both Delhi Kids underwent ASD surgical closure by open heart surgery.
PDA (Patent Ductus Arteriosus) Device Closure (Angiographically without Heart Surgery)
PDA device closure done angiographically without surgery (Child is from Sonipat, Haryana and from Ghaziabad, Uttar Pradesh respectively).
Balloon Dilatation of Coarctation of Aorta
34 months old male child successfully underwent “Balloon dilatation” of severely blocked segment of aorta known as “critical coractation of aorta”. Patient came from Bihar, India.

PDA DEVICE CLOSURE
15 months old female child from Dehradun city (uttarakhand) came for PDA device closure

TETRALOGY OF FALLOT (TOF) REPAIR
An extremely sick child from Nepal underwent successful TOF surgical repair

ASD SURGICAL CLOSURE
An African child underwent successful ASD surgical closure
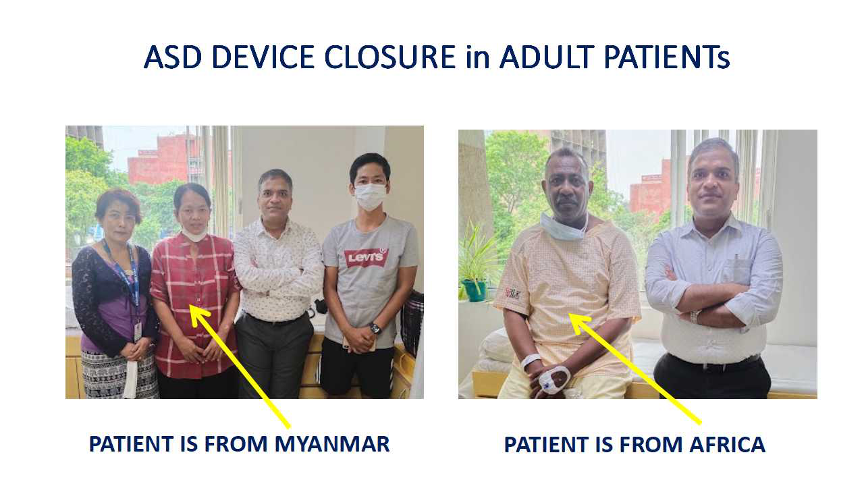
ASD Device Closure
Two adult patient underwent successful ASD device closure without open heart surgery
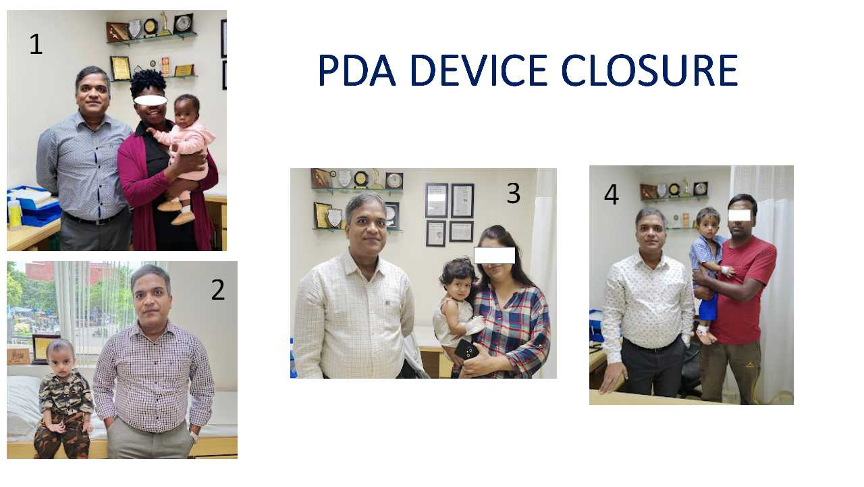
PDA Device Closure
1: A five months old child from Africa underwent successful PDA device closure
2: Underwent successful PDA device closure
3: Bengaluru child underwent successful PDA device closure
4: Delhi child underwent successful PDA device closure

Re-do Surgery for RV-PA conduit replacement
- An international child came with history of chortness of breath on exertion.
- Child underwent TOF repair with RV-PA conduit replacement at 1 year of age.
- Now presented with severely stenosed conduit.
- Underwent successful replacement of RV-PA conduit
- Courtesy: Dr Ramji Mehrotra, MS, McH, Cardiac surgeon

5 years old child underwent “AP Window Surgery”
- 5 years old girl child was diagnosed as a case of large AP window (2.8 cm) recently.
- Was having recurrent cough & cold in first year of life but not diagnosed as a case of congenital heart disease.
- Child underwent CT angio as well as Cardiac cath angiography before surgery for assessing whether child is still operable or not.
- After assessment, child underwent high risk AP Window Closure Surgery and discharged on 4-5th post-operative day.
- On follow up child is doing well.
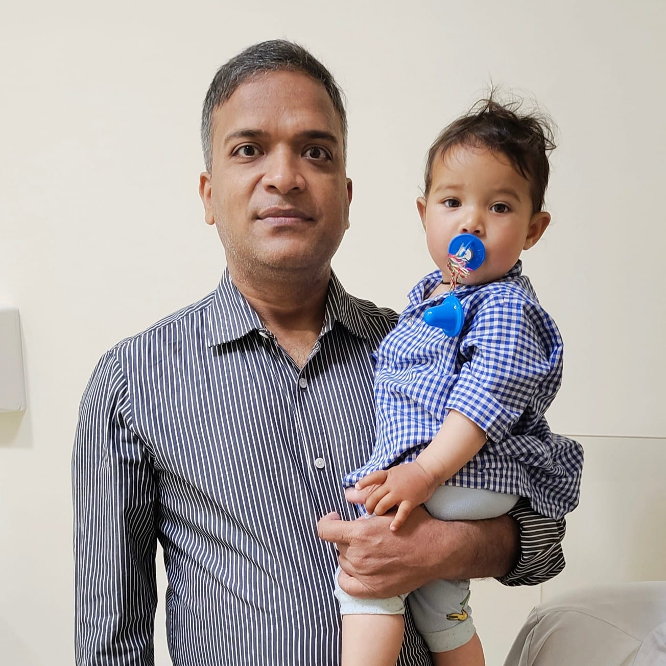
“PDA device closure” of a one year old child
- One year old child came with history of recurrent cough & cold since birth.
- Diagnosed as a case of Moderate sized “Patent Ductus Arteriosus (PDA)” with dilated left sided chambers of heart.
- PDA was closed by putting a device across the hole by angiograpgy without open heart surgery in cath lab
- Child was discharged next day and now symptoms free.

PDA Closure at 5 years of Age on a follow up child since the age of 6 months
Mesmerizing Experience:
- This child came in 2017 at 6 months of age for PDA ligation at BLK-MAX hospital from Zimbabwe. PDA was large in size with severe PAH like situation was there. It was not clear why PDA is having severe PAH (Eisenmenger like?), we evaluated child for sleep apnea in view of Down's syndrome. Child was suffering from Severe Sleep Apnea (OSA).
- Nasal CPAP was given and at 5-6 years of age, PAH decreased significantly.
- PDA ligation (via surgery) was done and now child is doing extremely good and lung pressures decreased significantly.
- Patient went back to Zimbabwe.

“VSD device closure” of an Iraqie Child
- 12 years old child came with diagnosis of moderate sized subaortic VSD with no complaints.
- VSD was closed by putting a device across the hole by angiograpgy without open heart surgery in cath lab
- Child was discharged next day with no complications.

“PDA device closure” of a 6 months old child
- 6 months old child came with history of poor weight gain since birth.
- Diagnosed as a case of Moderate sized “Patent Ductus Arteriosus (PDA)” with dilated left sided chambers of heart.
- PDA was closed by putting a device across the hole by angiograpgy without open heart surgery in cath lab
- Child was discharged next day and now gaining weight.

“ASD device closure” on a 5 year old child
- 5 years old male child came with diagnosis of large atrial septal defect (ASD) in the heart.
- He was evaluated and diagnosed as a case of large sized “Atrial Septal defect” with dilated right sided chambers of heart.
- ASD was closed by putting a device across the hole by angiograpgy without open heart surgery in cath lab
- Child was discharged next day and doing well.

Mesmerizing Experince while seeing this child
Amazing experience when I see this child
Came to us in respiratory failure in 2017 March, diagnosed as a case of severe form of Dilated Cardiomyopathy with heart pumping of 10 percent, Intubated and ventilated, lost hope that child will survive but God was watching team efforts...
Now child got complete normal form of heart function after 4 and half years of continuous treatment and finally discharged from follow up
This is a miracle for our team.

“PDA device closure” on an 11 months old child
- 11 months old child from “Uttar Pradesh” came with history of poor weight gain since birth.
- Diagnosed as a case of Moderate sized “Patent Ductus Arteriosus (PDA)” with dilated left sided chambers of heart.
- PDA was closed by putting a device across the hole by angiograpgy without open heart surgery in cath lab
- Child was discharged next day and doing well.

“PDA device closure” on a 13 months old child
- 13 months old female child came with history of poor weight gain since birth.
- Diagnosed as a case of Moderate sized “Patent Ductus Arteriosus (PDA)” with dilated left sided chambers of heart.
- PDA was closed by putting a device across the hole by angiograpgy without open heart surgery in cath lab
- Child was discharged next day and doing well

Life Saving “Balloon Aortiv Valvuloplasty” procedure on a 2 days old baby
- 2 days old sick newborn
- Came into shock like state with difficulty in breathing, decreased urine output, poor feeding
- Diagnosed as a case of “Critical Valvular Aortic Stenosis (Valvular AS) with poor heart pumping” due to deformed aortic valve
- Emergency “Balloon Aortic Valvuloplasty (BAV)” done without open heart surgery in cardiac cath lab
- Discharged on 2nd day of procedure in stable state with good pumping of heart as well as well opened narrowed aortic valve.

Life Saving “Balloon Atrial Septostomy (BAS)” procedure on a 16 days old blue baby
- 15 days old newborn who was deeply blue and in shock like state and was not maintaining proper oxygen flow in the whole body.
- Diagnosed as a case of complex cyanotic heart diseases (transposition of great vessels, d-TGA with no VSD/PDA and restrictive PFO).
- Emergency Procedure done in the form of “Balloon Atrial Septostomy (BAS)” that opened the narrowed PFO.
- Immediately after procedure, oxygen concentration in blood rose and shock like state disappear in few hours.
- Few days later, baby underwent surgery known as Arterial Switch Operation (ASO).
- Now, Baby is doing well.

Life Saving “Pericardiocentesis” procedure on a 8 years old child
- 8 years female child who came with history of shortness of breath for last few days that was rapidly progressive.
- Diagnosed as a case of massive fluid collection around heart (cardiac Temponade or massive pericardial effusion).
- Emergency, pericardiocentesis (pericardial tapping) was done that removed all collected fluids and patient clinically improved and discharged next day
- Diagnosed as a case of Tubercular pericardial effusion (TB pericardial effusion).

“PDA device closure” on a one year old child
- One year old female child came with history of poor weight gain since birth.
- Diagnosed as a case of Moderate sized “Patent Ductus Arteriosus (PDA)” with dilated left sided chambers of heart.
- PDA was closed by putting a device across the hole by angiograpgy without open heart surgery in cath lab
- Child was discharged next day and doing well and gaining weight now.

- Male child who was on follow up since birth
- Diagnosed as a case of “severe form of aortic valve stenosis” due to deformed bicuspid aortic valve (BAV).
- Underwent balloon dilatation of aortic valve (Balloon Aortic Valvuloplasty) at 1.5 months of age.
- Now child is 7-8 months of age and is doing well on follow up

6 year girl underwent “difficult PDA device closure” and discharged in 15-18 hours after the procedure.

Saved a sick newborn from life threatening heart rhythm disorder
Supraventricular Tachycardia
- 16 days old baby came on ventilator in sick state.
- His heart rate was more than 300/min (normal is less than 160/min).
- Echocardiogram showed very poor heart pumping.
- ECG was done which showed signs of pre-excitation (WPW syndrome).
- Baby was managed with IV medications (adenosine etc) but not responding.
- DC cardioversion was done which was also not responsive.
- Then multiple medicines were tried but all failed
- IV Metoprolol was started for a long duration and now baby responded very well.
- Patient discharged in 5-6 days and on follow-up, he is on medicines and is gaining weight with normal sinus rhythm in ECG.

Bringing back a hearty smile
Dilated Cardiomyopathy with Cardio-respiratory failure
- 6 months old male child came in very sick condition with air hunger and difficulty in breathing.
- He was diagnosed a case of severe left heart failure (Dilated Cardiomyopathy).
- Immediately, child was admitted in PICU and intubated and ventilated.
- Echocardiogram done which showed very poor heart pumping.
- Child was treated with diuretics, inotropes etc.
- His disease course was very fulminant and chances of recovery were very poor as child was not responding to medicines.
- But fortunately, he recovered, and discharged in 2 weeks.
- On follow-up, he gained weight with normal heart pumping (took almost 2 years for recover).

Tricuspid atresia heart disease
- Tazakistan (Russian) patient underwent successful Fontan operation at BLK hospital for tricuspid atresia (Cyanotic congenital heart disease).
- He came with history of increasing bluishness of lips and fingers (cyanosis).
- He underwent Glenn operation few years back for single ventricle pathway.
- After detailed evaluation, child underwent Pre-Fontan Cath study, and found suitable for Fontan operation.
- Same was done and patient discharged on 5th day after operation and doing well on follow up.

Balloon Dilatation of Coarctation of Aorta
- 10 year old male child from “CONGO” came with history of frequent leg pains while walking.
- On examination, his lower limb pulses were absent along with systolic murmur all over the chest.
- On evaluation, child was having “severe Coarctation of Aorta” (COA) with unicuspid aortic valve with “Severe Aortic Stenosis” (AS) on echocardiogram. Aortic valve was not in proper position, it was prolapsed.
- Probably there was a Ventricular Septal Defect (VSD) that was closed by prolapse of aortic valve.
- Family was counselled regarding the requirement of immediate ballooning of narrowed blood vessel (aorta, coarctation of aorta segment) leaving aortic valve for surgical palliation.
- Aortic Valve Ballooning was deferred as it was prolapsed and while doing balloon dilatation, it may leak severely and lead to emergency like situation to the child.
- After taking written consent, child was taken to cardiac cath lab for Ballooning of coarctation of aorta.
- He underwent above mentioned procedure successfully with no complications.
- Narrowed segment of Aorta opened well and there were good pulses in both limbs.

VSD Device Closure
- 4 years “Russian” girl child came with history of abnormal heart sound in chest (murmur).
- On evaluation, child was having an abnormal heart sound (pansystolic murmur in left lower chest).
- Echocardiogram showed a moderate sized “Ventricular Septal Defect (VSD)” with dilated LV (dilated cardiac chambers).
- On evaluation, VSD was suitable for closure by angiographic technique (VSD device closure).
- She underwent VSD device closure and discharged on next day with normal ECG.
- She was kept on oral aspirin tablet for six months.
- As per her translator, she is doing well in her home country.

ASD Device Closure
- 6 years girl child came with history of abnormal heart sound in chest.
- On evaluation, child was having an abnormal heart sound (wide and fixed spilt second heart sound).
- Echocardiogram showed a large Atrial Septal Defect (OS-ASD) with dilated RA/RV (dilated cardiac chambers).
- ASD was suitable for closure by angiographic technique (ASD device closure).
- She underwent device closure and discharged on next day.
- She was kept on oral aspirin tablet for six months.
- Now, after more than twelve months, she is gaining weight and doing well on follow-up.

VSD Surgical Closure
- “African” child, who came with history of very low weight and breathing difficulty since birth.
- Echocardiogram showed large ventricular septal defect (VSD).
- Underwent successful VSD surgical closure.
- On follow-up, she is doing good with normal weight gain.

VSD Surgical Closure
- “Russian” child came with history of increasing breathing difficulty since birth.
- On evaluation, child was having large VSD (Ventricular Septal Defect).
- Child underwent surgical closure of hole.
- Child is doing well on follow-up.

VSD Surgical Closure
- “African” female child (one year) who came with history of poor weight gain since birth.
- Her weight was poor and not able to walk and stand as well.
- Her ECG and chest x ray were normal.
- Echocardiogram showed a large ventricular septal defect (VSD) with dilated left atrium and left ventricle.
- As child was having low weight, there is high risk involved and after taking written informed consent, child was taken for open heart surgery.
- She was discharged in 5-6 days
- She is in constant touch with phone from her home country and now she is doing well and gaining weight.

ASD Surgical Closure
- 4 year female child who came with history of abnormal heart sound in chest
- Echocardiogram showed a large Atrial Septal Defect (OS-ASD) with dilated RA/RV (dilated cardiac chambers).
- Her ASD rims were deficient so plan was made to close ASD by surgical method.
- Open heart surgery was deferred in view of girl child so MICS surgery was planned.
- Minimal invasive cardiac surgery (MICS-ASD closure) was done
- In MICS surgery, there will a very little scar on right side of the chest (not in midline)
- She was discharged after 4 days of surgery.
- She is gaining weight and doing well on follow-up.

Balloon Pulmonary Valvuloplasty (BPV)
- 5 kilogram female child who was having moderate sized Atrial septal defect with small ventricular septal defect (ASD and VSD) along with severe narrowing in Pulmonary Valve (pulmonary stenosis),
- Her vitals were stable with normal saturation.
- Echocardiogram showed severely obstructed pulmonary valve (severe valvular pulmonary stenosis) that required immediate balloon dilatation of pulmonary valve in cardiac cath lab (known as Balloon Pulmonary Valvuloplasty; BPV).
- Plan was made and discussed with family that we will do only BPV and will not touch ASD & VSD as these will not cause any harm as of now.
- After taking informed written consent, child was taken to cath lab and by angiographic technique; her pulmonary valve was opened by using a balloon.
- Post-procedure, child remained stable.
- His ASD and VSD remained as such and now she is very well on follow-up.
- Last follow-up showed well opened pulmonary valve with mild pulmonary regurgitation.

Device Closure of PDA
- 8 months male child came with history of poor weight gain since birth.
- His vitals were normal
- There was a continuous murmur in chest while examining the child.
- ECG and chest X ray were suggestive of dilated left ventricle.
- Echocardiogram was done which showed moderate sized “Patent Ductus Arteriosus (PDA)”.
- Family was counselled regarding the requirement of PDA closure by device technique without open heart surgery.
- He underwent PDA device closure and was discharged on next day.
- He was not advised any medicines after the procedure.
- Now, after more than eighteen months, he is gaining weight and doing well on follow-up.

Pericardiocentesis
- 4 year old girl child who was having history of fever with mild cough and cold.
- Her vitals were stable.
- Chest X ray showed large cardiac shadow.
- ECG was suggestive of pulsus alternans.
- Echocardiogram done which showed massive collection around the heart (pericardial temponade).
- Family was counselled regarding the urgent removal of collection around the heart (Pericardiocentesis).
- Child was taken to cath lab (without open heart surgery) for drainage of collection under fluoroscopic and echo guidance.
- Approximately 250 ml straw coloured fluid was aspirated and that came out
- Child was treated with steroids and anti-tubercular medicines (ATT) and now after 6 months, ATT stopped
- Repeat echocardiogram did not show any signs of constriction around the heart.

Balloon Pulmonary Valvuloplasty (BPV)
- 11 months “CONGO” child came with history of abnormal sound in chest with the diagnosis of narrowing in pulmonary artery (pulmonary stenosis).
- His vitals were stable with normal saturation.
- Echocardiogram done which showed severe narrowing in pulmonary valve (severe pulmonary stenosis) that required immediate balloon dilatation of pulmonary valve in cardiac cath lab (known as Balloon Pulmonary Valvuloplasty; BPV).
- After taking informed written consent, child was taken to cath lab and by angiographic technique; his pulmonary valve was opened by using a balloon.
- Post-procedure, child remained stable and is on regular follow-up.
- Last follow-up showed well opened pulmonary valve.

ASD Device Closure
- 10 years, 15 kilogram child from Jammu, India came with history of poor weight gain.
- On evaluation, child was having an abnormal heart sound (wide and fixed spilt second heart sound).
- Echocardiogram showed a large Atrial Septal Defect (OS-ASD) with dilated RA/RV (dilated cardiac chambers).
- ASD was suitable for closure by angiographic technique (ASD device closure).
- She underwent device closure and discharged on next day.
- She was kept on oral aspirin tablet for six months.
- Now, after more than twelve months, she is gaining weight and doing well on follow-up.

Waiting for the right time
- 6 months “African” child came for closure of PDA.
- On evaluation, child was having features of Down Syndrome with laboured breathing and saturation of 75% in both upper and lower limbs with prominent heart sounds (loud S2).
- On echocardiogram, child was having moderate sized PDA with severe increase in lung pressures (Pulmonary Arterial Hypertension, PAH).
- Child was admitted in view of difficulty in breathing and kept under ICU care.
- On further evaluation, child was having snoring and diagnosed as a case of sleep apnea with obstructed airways (OSA).
- Child kept on CPAP support (non-invasive) ventilation for a long time and discharged on Bi-PAP support
- PDA was not closed in view of high lung pressures.
- Child is on regular follow-up for last two years and now off Bi-PAP support (child is on room air) and now his PDA is shunting mainly in favourable direction.
- Further plan is to close the PDA in follow-up depending on his lung pressures.

Bringing back a hearty smile
PDA LIGATION
- Preterm 1.2 kilogram baby referred from another hospital on non-invasive ventilatory (CPAP) support.
- Child was tachypneic (breathing difficulty), having rapid heart rate.
- Chest X ray showed increased lung vascularity (pulmonary plethora)
- ECG was non-conclusive.
- Echocardiogram done which showed Large Patent Ductus Arteriosus (PDA) of size 4.5 mm with enlargement of left atrium and left ventricle (dilated cardiac chambers).
- After counselling the family regarding the necessity of PDA closure by surgical method (PDA ligation), baby was taken for the surgery.
- Surgery was done and child remained stable in next 2 days and discharged in next few days.
- On follow up, now the child is one year 5 months and is gaining weight.

Getting freedom from pain in lower limbs
Balloon Dilatation of Corctation of aorta with VSD device closure
- 7 year child from Uzbekistan came with history of frequent leg pains specially on running and playing.
- On examination, his vitals were stable with pansystolic murmur (abnormal heart sound heard on chest during examination). There were weak pulses in bilateral lower limbs.
- On evaluation, child was having moderate sized “Ventricular Septal Defect” with severe “Coarctation of Aorta” (VSD with COA) on echocardiogram.
- His chest X ray and ECG were normal for the age.
- Family was counselled regarding the requirement of immediate ballooning of narrowed blood vessel (aorta, coarctation of aorta segment) along with VSD closure by angiographic technique (VSD device closure).
- After taking written consent, child was taken to cardiac cath lab for Ballooning of coarctation of aorta followed by VSD device closure in the same sitting.
- He underwent above mentioned procedure successfully with no complications.
- Post procedure, child was kept on oral medicine (Aspirin) for 6 months.

Post Glenn Operation
- 11 months old male child from IRAQ underwent successful Glenn Shunt in Dec 2019
- Child was having single ventricle physiology
- He underwent BT shunt surgery at the age of 2 months
- He recovered well and now is free from symptoms currently
- He shall need Fontan surgery between 3-4 years of age or earlier if required.

Atrial Septal Defect surgery
4 year male child who came with complaints of poor weight gain. On evaluation, he was having a large Atrial Septal Defect (ASD) with very poor margins all around with dilated heart chambers. Family was counselled in detail regarding the requirement of surgery for ASD. ASD surgery was done through midline. Child was discharged on 4th post-operative day in stable state. On follow-up, child is doing well and now gaining weight.

Recovered from Dilated Heart (DCM)
- 3 months male child successfully treated for dilated cardiomyopathy (DCM)
- Left sided heart was hugely dilated
- Child was in respiratory distress when came to the emergency
- Treated for 5-6 days in ICU
- Now all medicines are stopped and child is growing well

VSD Device Closure of “Congo Child”
- 9 years old Congo child underwent successful VSD device closure in March, 2020
- Came with Small to moderate sized VSD along with significant LV to RA shunt
- Advised to close the VSD in view of significant LV-RA shunt (Gerbode defect)
- VSD was suitable for closure by angiographic method (commonly known as Laser technique/device closure technique)
- Closed with ADO I device (10*8 mm in size)
- Post device, ECG remained normal and discharged on next day
- Currently she is well with no problems related to ECG etc.

Atrial Septal Defect (ASD) Device Closure
- 11 years male child came with history of occasional breathing difficulty for last few years
- Diagnosed as a case of small ASD in one of the city of Uttar Pradesh
- Evaluated and diagnosed as a case of 2.7 cm secundum ASD
- Closed with 3 cm ASD device by LASER technique (without surgery)
- Doing well and free from symptoms

