AP window diagnosis – Blog
AP Window can be diagnosed even before delivery of the baby by doing Fetal Echocardiogram test but sometimes, it can...
Read More
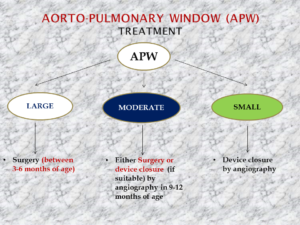
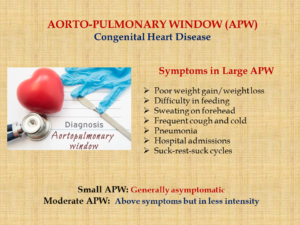
AORTO-PULMONARY WINDOW (AP Window)
Aorto-pulmonary Window (AP Window) is a very form of congenital heart defect (CHD), meaning by present at birth. In AP...
Read More
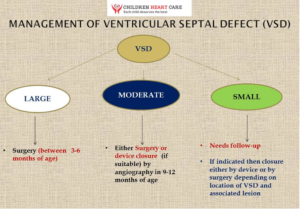
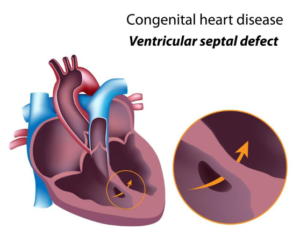
What is the treatment of VSD?
Treatment of VSD depends on the size of the VSD as well as age and weight of the child. Small...
Read More
How VSD is diagnosed (Ventricular Septal Defect diagnosis)?
Antenatal testing by doing “fetal echocardiogram” can let us know about ventricular septal defect even during pregnancy even before delivery...
Read More
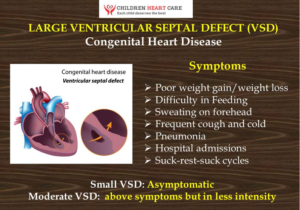
Symptoms Due to Ventricular Septal Defect (VSD)
The signs and symptoms of VSD vary and it depends mainly on the size of the VSD (hole). If the...
Read More
Ventricular Septal Defect (VSD) – Blog
VSD is a form of hole in the wall of heart that is situated between two lower chambers of the...
Read More
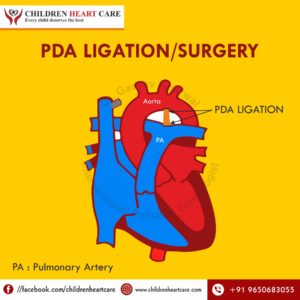
TREATMENT OF PATENT DUCTUS ARETRIOSUS (PDA)
Treatment options for PDA? Preterm babies (immature babies) PDA can be treated by giving medicines like paracetamol or brufen along...
Read More
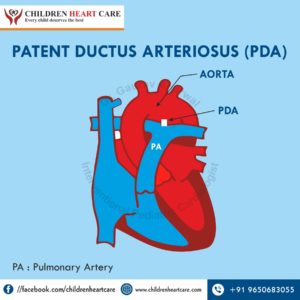
PATENT DUCTUS ARTERIOSUS (PDA) IN CHILDREN
What is Patent Ductus Arteriosus (PDA)? This is a hole that is normally present when the child is in mother’s...
Read More
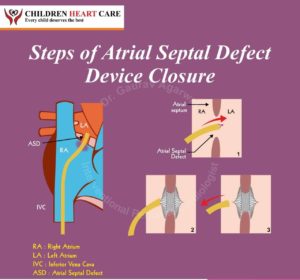
Treatment of Atrial Septal Defect (ASD) – Blog
There is no role of medicines in closing or treating the atrial septal defects (ASD). Only ostium secundum (OS-ASD) with...
Read More
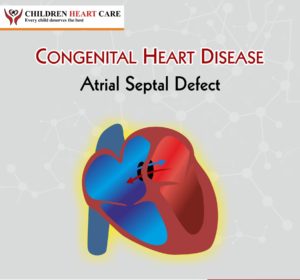
ATRIAL SEPTAL DEFECT (ASD) – Blog
Atrial septal defect is a congenital heart defect (CHD). This is in the form of a hole between two upper...
Read More
HYPERTROPHIC CARDIOMYOPATHY (HOCM)
Hypertrophic cardiomyopathy (HCM/HOCM) is characterized by thickening of heart walls with no cause clinically. This can results in poor capability of...
Read More
INFECTIVE ENDOCARDITIS (IE)
Infective endocarditis refers to infection of heart endocardium mainly the valves. It can affect various organs of the body like...
Read More
RHEUMATIC HEART DISEASE (RHD)
It is characterised by damage of heart structures by Rheumatic fever. Generally affected cardiac structures are mitral and aortic valves....
Read More
Long QT syndrome (LQTS)
Long QT syndrome (LQTS) is characterized by abnormality in repolarization of the heart leading long QT interval. Long QT can occur...
Read More
SINGLE VENTRICLE
Single ventricle means that one of two ventricles (lower chambers of heart) is very small in size. Examples of single...
Read More
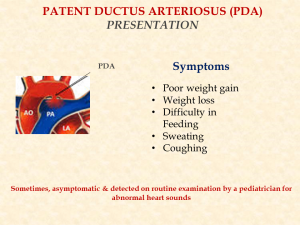
PDA Presentation
It depends on age, maturity of newborn, weight of baby and the size of PDA. Preterm Babies: Preterm babies especially...
Read More
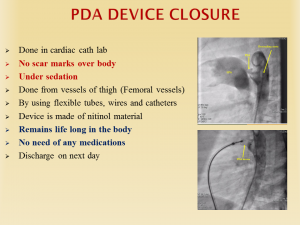
PDA Management
PDA treatment in babies depends on maturity level and weight of babies. Preterm babies needs conservative followed by drug treatment...
Read More
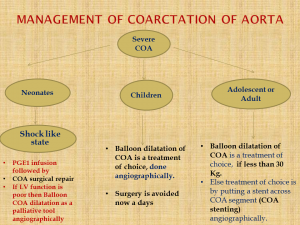
Management of Coarctation of aorta (COA)
Coarctation of aorta can be managed either by drug treatment or by balloon dilatation/stenting in cath lab or by surgery....
Read More
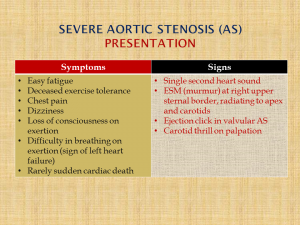
Presentation of Severe Aortic Stenosis (AS)
There is a great vessel in heart known as aorta which supplies pure blood to different parts of the body....
Read More
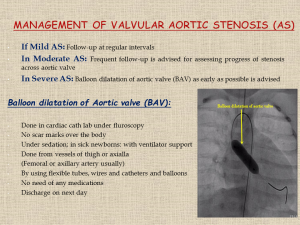
Management of Valvular Aortic Stenosis (AS)
Treatment depends on “age of presentation” as well as on “severity of obstruction”. Newborn babies with severe aortic stenosis are...
Read More